Flu Season Is Coming. Is Your Practice Ready?
As we continue to look for silver linings from the yearlong-plus pandemic, there’s one that stands out: Seasonal influenza infections all but disappeared. This was thanks in large part to all the new behaviors we were forced to adopt to stop the spread of COVID-19: staying home, social distancing, wearing masks, and increased hand-washing.
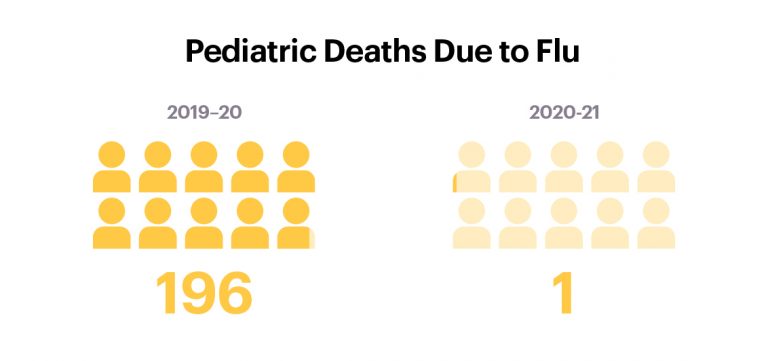
According to the Centers for Disease Control and Prevention (CDC), there were only 2,038 flu cases during the season (Sept. 27, 2020 to April 24, 2021), compared with an estimated 38 million cases during the 2019–20 season. The hospitalization rate for the 2020–21 U.S. flu season was just 0.7 per 100,000 people—the lowest since the agency started tracking flu data back in 2005. And there’s one more piece of significant news: During last year’s flu season, there was just a single pediatric flu death, compared with 196 during the 2019–20 flu season.
“Prior to last year, influenza in the United States was responsible for more pediatric deaths than any other vaccine-preventable disease” says Joseph Bocchini, MD, FAAP, Director of the Willis-Knighton Health System Children’s Services and the Department of Pediatrics at Tulane University. Most of the children who died had no underlying condition known to increase the risk of complications of influenza, and most were unvaccinated.
But don’t get too comfy. Experts say the respite from influenza cases we experienced last year could actually mean stormier weather for the coming 2021–22 flu season.
An Especially Unpredictable Flu Season
The first reason: Infection numbers were so low last year, scientists don’t have enough applicable data to predict what flu strains will be predominant this year. Without this valuable data, researchers will have a harder time creating effective vaccines for this year’s flu.
When they met to discuss the upcoming season, the World Health Organization (WHO) recommended vaccine manufacturers create a flu vaccine similar to last season’s, specifically keeping two B strains (representing the dominant strain in most of the globe) and changing out two A strains of the quadrivalent vaccine for the upcoming season. Here’s why: fewer flu infections last year means there were fewer virus specimens for researchers to use to create the upcoming year’s vaccines. But from this smaller pool, they saw continued efficacy from last year’s B strains; less so with the A strains. So for this year, they updated the A strains while leaving B strains basically untouched.
The Danger of "Pandemic Fatigue"
The second reason this upcoming flu season could be worse is complacency due to “pandemic fatigue.” After the 1918 flu pandemic, people came out in full force to gather, mingle, hug, and kiss, leading to what became known as “the roaring ‘20s.” As our own pandemic restrictions start lifting, we’re likely to experience something similar and create a scenario where the influenza virus can thrive. As we decrease mitigation strategies to control COVID-19, children will again be at risk for influenza in school (where many community flu outbreaks begin) and if infected, will bring the virus home to their parents. Many adults have underlying conditions which can worsen influenza infections and lead to complications and deaths. (The vast majority of influenza deaths are adults.)
“We know social distancing stops flu, but we also know when you stop social distancing, the flu will come back,” says Litjen Tan, Ph.D., chief strategy officer for the Immunization Action Coalition. “Our job as people working in public health is to remind people to not get complacent; the ‘twindemic’ risk we were so worried about last year at this time has not gone away. Don’t think because there was no flu last year, there will be no flu this year. Flu always teaches us a lesson when we do that.”
"The 'twindemic' risk we were so worried about this time last year has not gone away."
- L.J Tan, Chief Strategy Officer
Immunization Action Coalition
Tan says a priority for his agency is helping to make sure that manufacturers bring enough vaccine doses to market this year. “Because there were so few cases last year, we have to reassure manufacturers that we will get these vaccines out to patients,” he says. “And we have to make sure physicians are spreading the word to their patients so we keep people protected and don’t waste valuable vaccine resources.”
There’s also an effort to make this year’s flu season an opportunity for double duty, making sure anyone who comes in to get a COVID-19 vaccination also gets the flu shot (and vice versa). Now that the CDC says that the two vaccines can be given at the same time, there is no need to wait two weeks between.
Applying Lessons Learned
Tan also encourages physicians to take advantage of the lessons we’ve learned from the COVID-19 vaccination distribution to create more opportunities for their patients to get vaccinated against the flu this year. “We had a massive rollout effort with the COVID-19 vaccine, so why not do something smaller in your healthcare system, like setting up a mobile flu clinic in your parking lot,” he says. “The idea is to keep awareness of the flu high in people’s minds so we can get more people vaccinated than ever. Providers are so important to this effort, especially to fight ‘pandemic fatigue.’ When a provider tells a patient, ‘OK, we’ve got you covered for COVID-19; you’re also due for flu,’ the patient usually goes ahead and gets it done. So having providers help get patients back into the system and making sure getting the flu vaccine is a priority for them, will be a huge help.”
"It is best to begin immunizing adults and children in September…[and] continue throughout the influenza season…as different types of influenza virus may come into a community through April or May."
- Joseph Bocchini, MD, FAAP
Director of the Willis-Knighton Health System Children’s Services and the Department of Pediatrics at Tulane University
Dr. Bocchini notes that it is important to have your patients vaccinated before the influenza season begins. “It is best to begin immunizing adults and children in September and plan your office immunization program to have everyone immunized by the end of October. However, vaccination should continue throughout the influenza season for persons not already immunized, as different types of influenza virus may come into a community through April or May.”
Administration Fees Remain Inadequate
From a cost perspective, this year continues the unwelcome trend of lower vaccine administration fees for practices who care for Medicare patients. Here’s a bit of history on the rollercoaster ride of admin fees: In the early 2000s, Medicare paid physicians between $2 and $3 per administered dose of flu vaccine, depending on the state. The immunization community rallied to raise it, and in 2006, Medicare brought the fee up to the low-to-mid $20s. Rates hovered there for about a decade, but then in 2017, Medicare altered the physician fee schedule, and vaccine administration fees plummeted. Today, the national average is about $17 per administered dose.
"Medicare’s flu vaccine administration fees remain below 2006 levels."
Tan’s agency has been on the frontlines, fighting to keep these fees from sinking any lower—and to get them back to the 2006 rates. “If these rates drop any lower, providers will start saying. ‘It’s not worth it; it costs too much money,’” Tan says, noting that it’s a hard battle, but “it’s something we’re going to keep working on.”
According to Tan, providers can play a role in this effort, too. If you’re part of a medical association, you can work with it to help make sure the pay rates don’t dwindle. You can also team up with the Adult Vaccine Access Coalition, an organization that’s doing plenty of work on this issue. “The more voices we have, the better,” he says.

Comments are closed