
Streamline claims workflows, improve productivity and facilitate faster reimbursement
Automation and Innovation Drive Efficiency and Faster Payments
Automating the revenue cycle end-to-end enables you to gain control of the financial aspects of your practice. Change Healthcare’s Revenue Performance Advisor helps you with every facet, from patient check-in to payment posting. Real-time visibility into eligibility, claim status, rejections and denials streamlines your workflow to facilitate fast reimbursement.
Our network connects you to 2,200-plus government and private payers so you can:
• Verify patient eligibility in real time, either at point of service or submit batch requests for the next day’s roster
• Give patients an estimate/ explanation of what they owe at the point of service to drive upfront collections and patient satisfaction
Claims that are validated and scrubbed before submission get paid faster
• Submit, track, and manage claims faster with advanced search functionality
• Create work queues to update groups of claims or one claim at a time, and assign tasks to others
• Print EOBs and view ERA matched to claims
• Identify gaps between submission and payment
Our solution leverages:
• Artificial intelligence and machine-learning technology to predict which claims are likely to be denied before they are submitted to the payer, so staff can make corrections upstream
• Real-time edits/corrections to rejections and denials for faster resubmission
• Pre-populated appeals letters
• Automatic detection of root issues
• Standardized formats to link original claims to adjudications
• Ability to easily prepare secondary claims based on initial file and primary ERA
Help improve financial performance through enhanced reporting:
• Actionable, real-time analytics drive informed, proactive decisions
• Real-time access to key performance indicators span the entire revenue cycle
• Customizable reports (40+) help identify problem trends before they impact the bottom line, e.g., ‘top ten rejections by payer’
• Performance can be measured throughout
the revenue cycle, e.g., clearinghouses, payers, peers, reimbursements, patient payments, and your practice
Here's how it works:
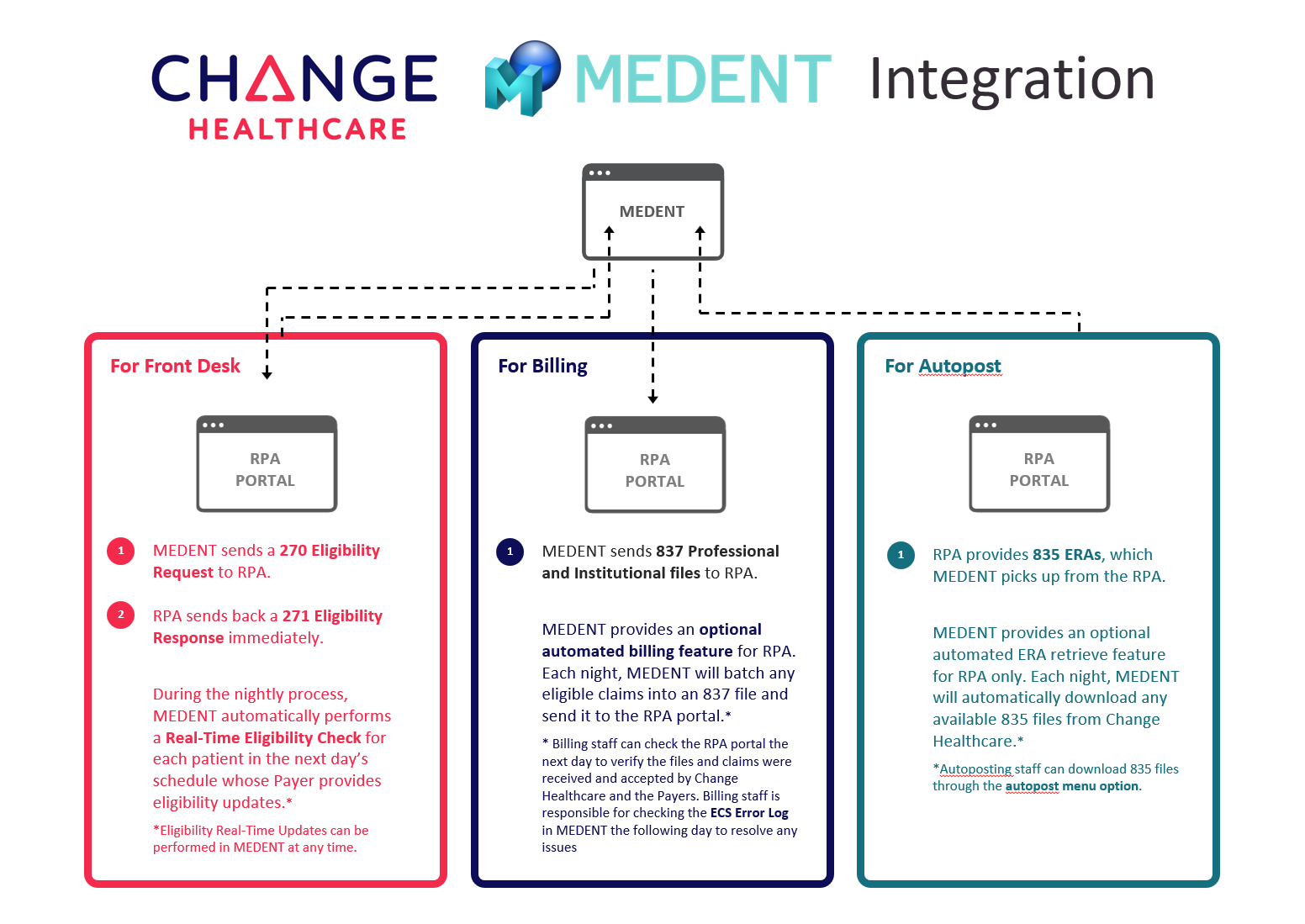
Optimize your revenue cycle from patient check-in to payment posting.
Our team is ready to get you started!
