“Many of the times, [the ePA] will be instant, so by the time the patient gets to the pharmacy, it’s already done and they can pick up their prescription.”
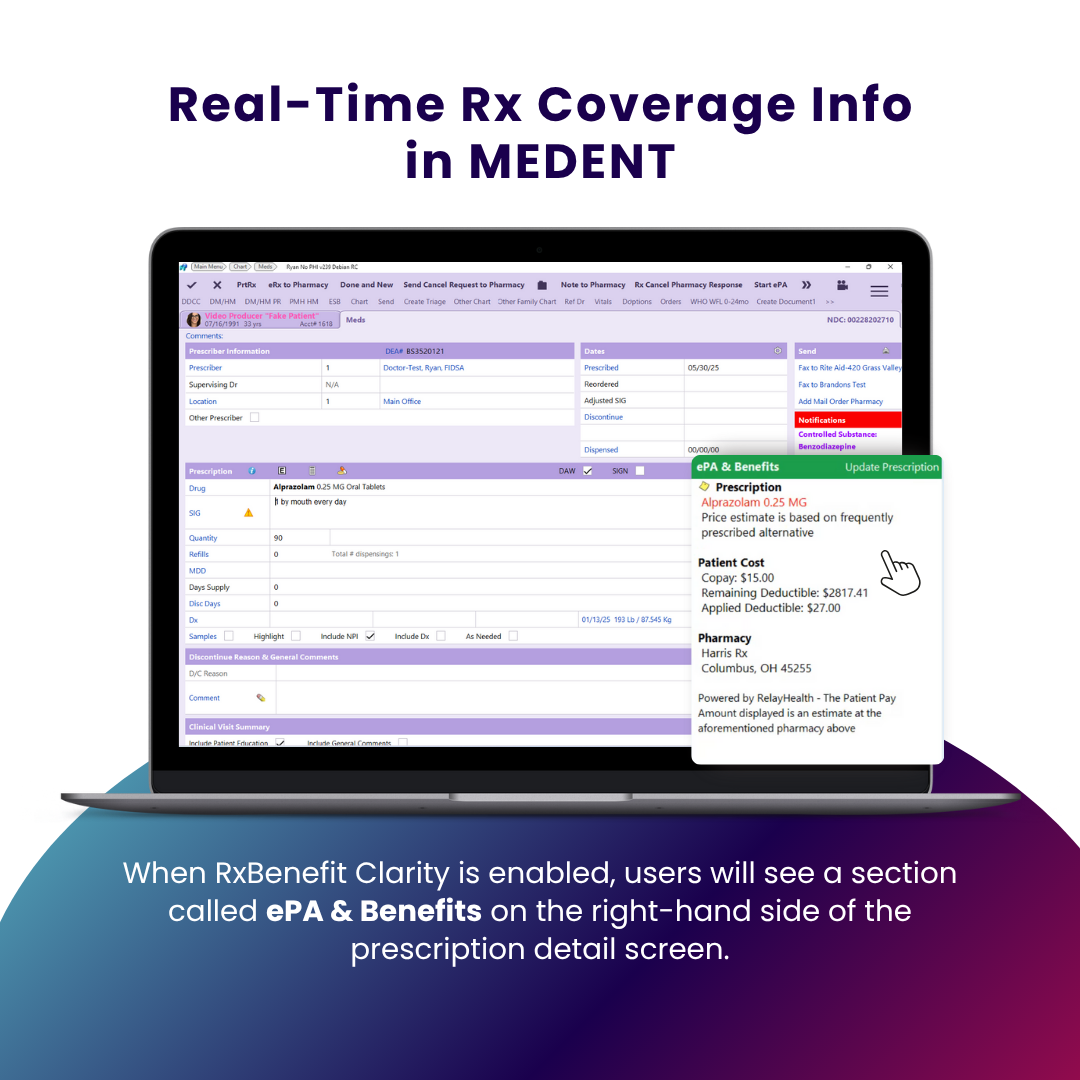
And with RxBenefit Clarity, you’ll see the patient’s out-of-pocket cost in MEDENT.
- Megan Chapman
- May 30, 2025
In today’s fast-paced healthcare environment, efficiency and accuracy are more important than ever. MEDENT is helping providers deliver better care with advanced tools that make the prescribing process faster, smarter and more transparent. With fully integrated ePrescribing, electronic prior authorization (ePA) and RxBenefit Clarity, MEDENT empowers providers to make informed decisions right at the point of care.
Smarter Prescribing with ePrescribing
Gone are the days of handwritten scripts and pharmacy callbacks. MEDENT’s ePrescribing feature allows providers to send prescriptions electronically, reducing errors and improving patient safety. Whether it’s a new medication or a refill, prescriptions are securely transmitted directly to the patient’s preferred pharmacy in seconds.
Key benefits include:
Seamless integration with MEDENT’s EHR, Patient Portal, Self Check-in Kiosk and Patient Pre-Check-In
Support for controlled substances (EPCS)
Allergy and interaction checks built into the workflow
Improved medication adherence and reduced phone tag with pharmacies
Speed Up Approvals with ePA
Waiting for prior authorization is frustrating for both patients and providers. With MEDENT and CoverMyMeds ePA, the process is streamlined into just a few clicks directly within the prescribing workflow.
Providers can:
Automatically check whether a prior authorization is required
Submit requests electronically in real time
Receive faster determinations, often within minutes
Minimize treatment delays and reduce administrative burden
“Historically, what’s happened is the script will be submitted to the pharmacy, the pharmacy submits the claim to the insurance company and the insurance company comes back and says a prior authorization is needed. The pharmacy then has to contact the practice and the provider and say, ‘We need a prior authorization for this.’ So now, you’ve got to start the prior authorization yourself,” said MEDENT Project Manager Matt Del Favero. “Because of the automated processes that CoverMyMeds has and the PBMs have, you may get a response in less than a minute, which is wonderful…Many of the times, it’ll be instant, so by the time the patient gets to the pharmacy, it’s already done and they can pick up their prescription.”
Price Transparency with RxBenefit Clarity
One of the most common reasons patients don’t fill prescriptions? Cost surprises at the pharmacy counter. MEDENT solves this with RxBenefit Clarity, a free, real-time benefit tool that gives providers visibility into:
Patient-specific out-of-pocket costs
Covered formulary alternatives
Pharmacy-specific pricing
Priori authorization or step therapy requirements
With this insight, providers can have cost-conscious conversations with patients and choose medications that are both clinically effective and financially accessible.
“If you’re a patient and you’re prescribed a medication and you don’t know what it’s going to cost you when you go to the pharmacy, you may not pick it up for that fear that it may cost you money or more than you expect,” Del Favero said. “If you have that information from the provider at the time it’s being prescribed, you know beforehand, ‘Yes, I can afford this.'”
Why It Matters
Combining these features into one cohesive system means fewer disruptions, reduced administrative work and a more seamless patient experience. Providers get real-time information, faster approvals and more prescribing power — all within the MEDENT platform.
Ready to sign up?
Contact us today to enable ePA and RxBenefit Clarity for FREE!
Listen to Episode 16 of our podcast, MEDENT Minutes, to hear how ePA & RxBenefit Clarity can help you streamline your workflow and improve medication adherence.