Imagine this…
It’s 8:15 AM at the front desk. The phone is ringing, patients are signing in and you’re juggling messages from providers. Then, you see it: the dreaded red “e” in Chart Central.
A patient’s insurance is inactive.
Now you’re scrambling to make calls, verify coverage and explain to the patient why their visit might not be covered. All of this while trying to keep the line moving.
This scenario happens far too often in medical offices. The problem isn’t just the stress; it’s the lost time, delayed check-ins, and increased risk of claim denials that come with last-minute eligibility surprises.
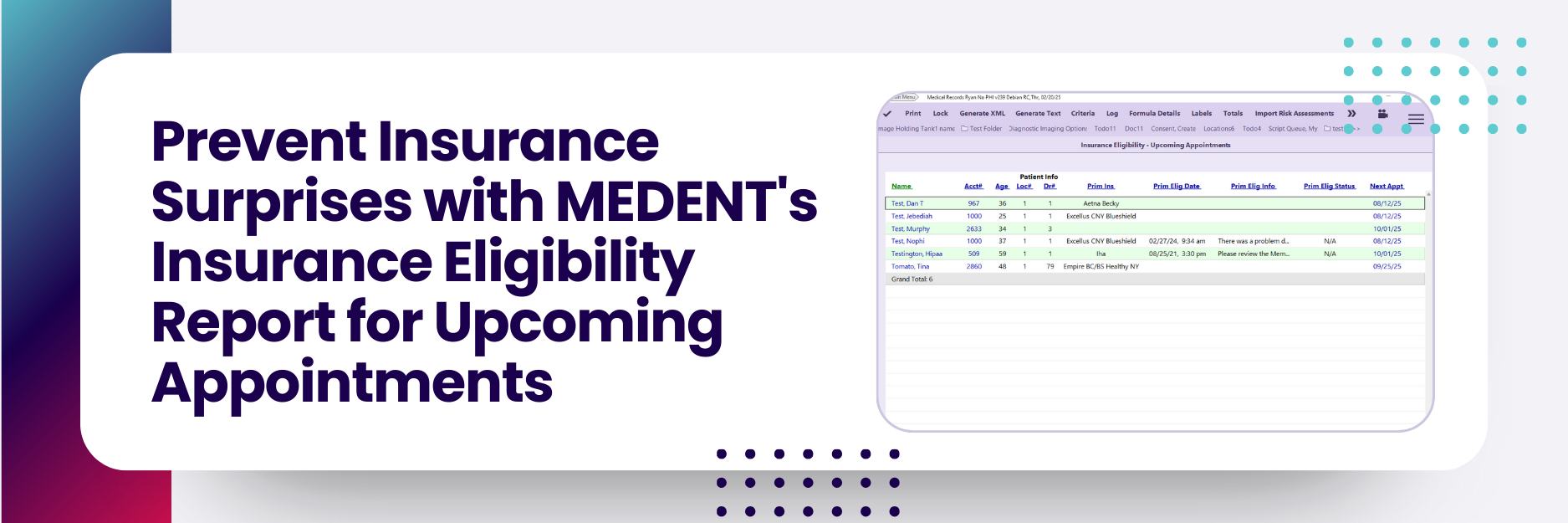
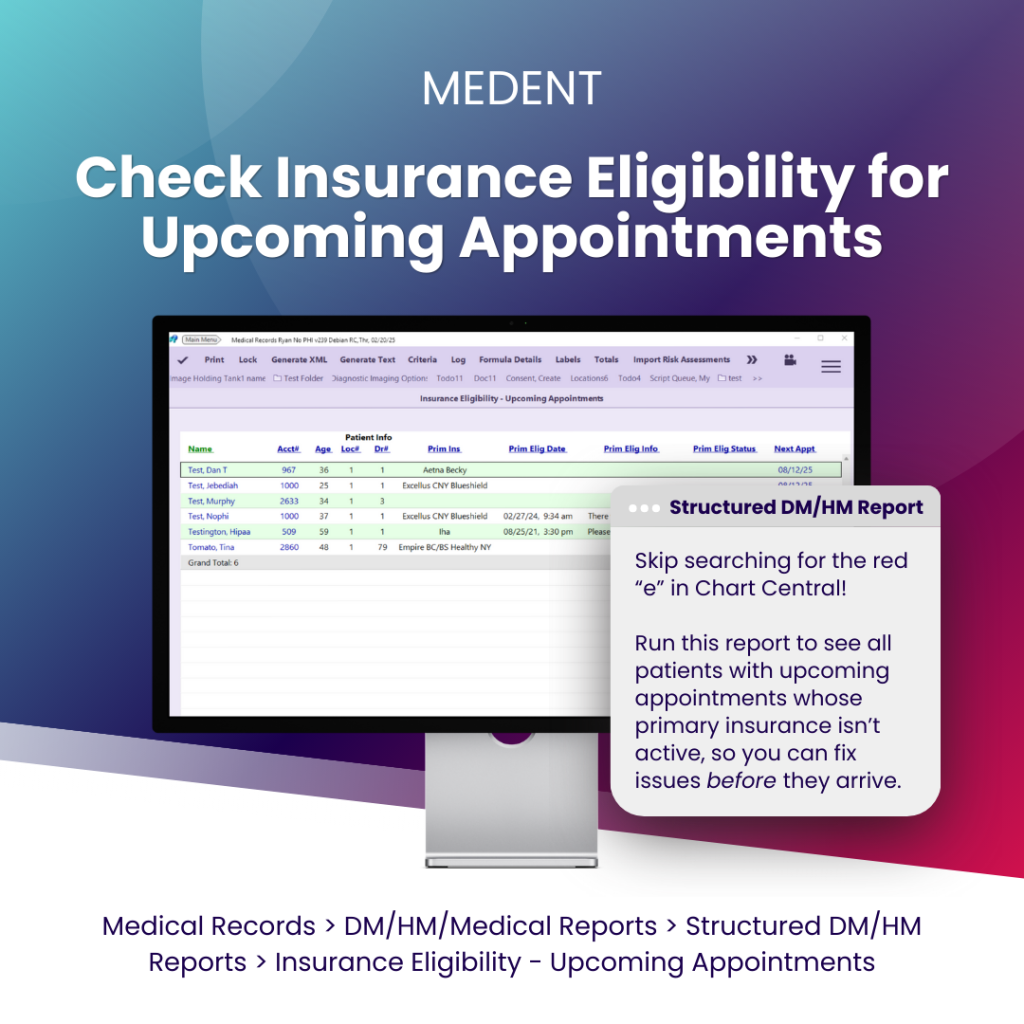
With MEDENT’s Insurance Eligibility – Upcoming Appointments report, your team can stop reacting and start planning.
Instead of scrolling through Chart Central for red and yellow “e” icons, this Structured DM/HM Report creates an interactive work bucket that shows all patients with upcoming appointments whose primary insurance is inactive or needs verification.
You can review this list days or even weeks in advance, giving your team time to:
Contact patients early to update coverage information
Verify benefits directly with the payer before the visit
Prevent claim denials by ensuring coverage is active before services are rendered
Saves staff time – No more hunting through individual charts
Protects revenue – Resolve insurance issues before they lead to unpaid claims
Improves patient experience – Smooth, fast check-in without awkward conversations about coverage
Supports proactive planning – Keeps schedules running efficiently and reduces morning chaos
By using the Insurance Eligibility – Upcoming Appointments report, your staff can spend less time on last-minute problems and more time focusing on what really matters: your patients.
Because mornings should start with coffee, not insurance surprises.